Release date: 2016-03-29
Dae-Hyeong Kim, an assistant professor at Seoul National University, was selected as the 2013 Global Outstanding Young Innovator by the MIT Technology Review magazine for his outstanding contribution to the use of stretchable materials for medical devices.
Gu Yu, assistant professor of the Department of Biomedical Engineering at the University of North Carolina's Chapel Hill School of Medicine, School of Pharmacy, North Carolina State University, was invented the "Intelligent Insulin Patch" by the MIT Technology Review. Selected as a global outstanding young talent in 2015.
These two young people from the Eastern world were 34 years old when they were selected as "outstanding young people in the world." Their leading research in the field of diabetes surveillance is highly regarded by journals such as Nature. If everything goes well, the health management of people with diabetes will be another story in the next 5 to 10 years.
Graphene wristband that monitors and regulates blood sugar levels
On March 21st, Nature and Nanotechnology magazine published the latest research by the Dae-Hyeong Kim team. The Kim team invented a graphene wristband that monitors and regulates blood sugar levels (1).
This wristband consists of two parts, one of which is the blood glucose concentration monitoring area and the other part is the treatment area (controlling blood glucose concentration).

Hui Won Yun-Seoul National University
Graphene has the reputation of being the king of new materials. Due to its high toughness, high light transmittance and good electrical conductivity, it has received a lot of attention in many fields in recent years. The Kim team also wants to use this new material in the medical field. However, the inherent inertness of graphene materials, that is, the lack of electrochemical capability, has also plagued many researchers. Kim then creatively blended graphene with gold. This small change made graphene a sensor that can detect skin temperature and humidity, sweat pH and glucose concentration. Finally, the blood glucose concentration is comprehensively analyzed based on the temperature and humidity of the skin, the pH of the sweat, and the glucose concentration. And pass the data to the mobile device.
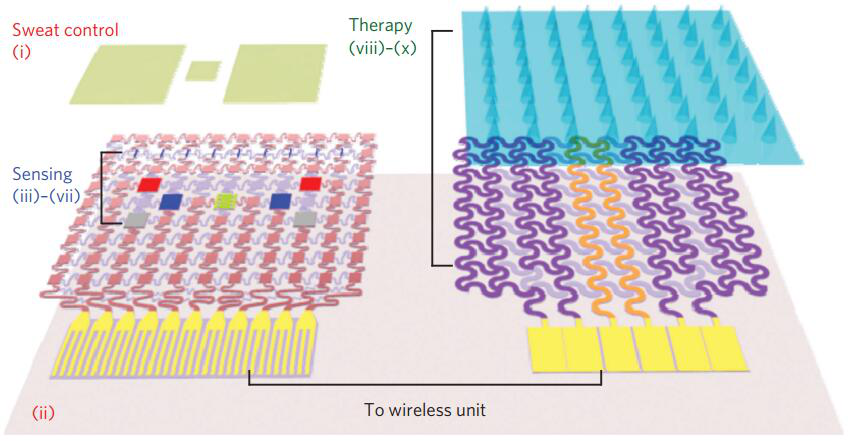
The monitoring area on the left and the treatment area on the right (1)
Once the monitoring area finds that the blood glucose concentration exceeds the standard, the heater located in the treatment area will activate the micro-needle to melt the outer membrane of the drug storage body, and the micro-needle will penetrate under the superficial skin to inject the hypoglycemic drug metformin into the patient. The purpose of controlling blood sugar. Of course, in order to avoid excessive hypoglycemic drugs injected into the human body, the melting of the meltable outer membrane on the surface of the needle in the treatment area is controlled in a time-sharing manner. The implication is that the fragments melt, and once the blood sugar is controlled, the melting stops. Ultimately achieve intelligent regulation of blood sugar concentration.
Can such a smart blood glucose management patch be available when it comes to market? I can't predict the exact time. But if you know that this device is jointly developed by the Kim team and MC10, a well-known flexible electronics company in Massachusetts, you will have more confidence in the time it will be available.
Smart insulin patch
Compared to the Kim team's combination of high-tech, and finally through the sweat to monitor the blood sugar concentration of the wristband, Gu Yu team's smart insulin patch is much more direct.
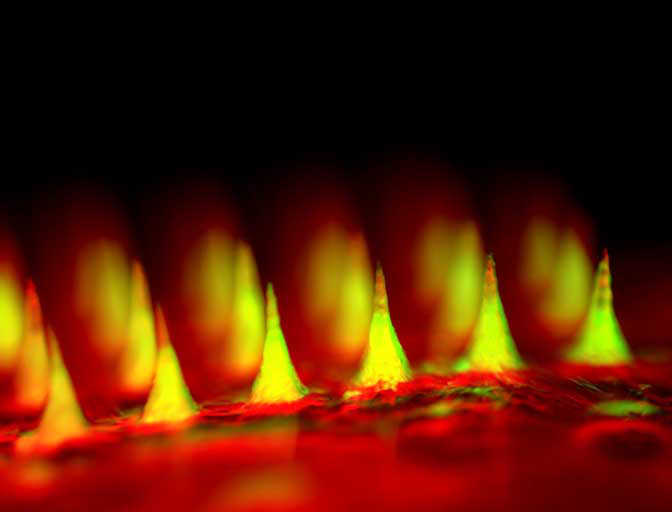
Smart insulin patch was named one of the top 10 most beautiful photos in 2015 by Science
The “smart insulin patch†developed by Gu Yu’s team is only the size of the fingernail, and the side of the patch is covered with 121 tiny needles filled with tiny vesicles. When the blood glucose level is too high, these vesicles will open and release insulin.
Schematic diagram of the working principle of the patch (2)
On July 7, 2015, the research results of the Gu Yu team were published on PNAS (2), and they quickly became the headlines of Nature and Science. It’s a big trend to end the era of diabetes injection therapy.
The principle of this intelligent insulin patch by Gu Yu team is very simple, but the design is very clever. They cleverly use the chemical reaction process in the body to achieve the purpose of releasing insulin. They also put hypoglycemic insulin in the microneedles of the patch, but this insulin is also wrapped in a chemical. When the blood glucose level rises, the glucose entering the microneedle from the blood will chemically react in the microneedle, causing the insulin-encapsulated vesicle to rupture and release the insulin. When the blood glucose level is lowered, insulin stops releasing. It also skillfully achieves controllable insulin release.

When you put it on your body, it is like this
In order to achieve more sustained blood sugar regulation, the Gu Yu team made further improvements to this smart insulin patch. This time, they replaced the insulin in the patch directly with beta cells that produce insulin.
The green color of the patch is the islet cells, and the orange color is the glucose sensor (3)
Transplantation of islet beta cells is actually a treatment for diabetes, but due to the rejection of allogeneic transplantation, this method can not meet the needs of all. This method of Gu Yu team effectively avoids rejection (because immune cells are isolated). In February of this year, the research results of the Gu Yu team were published in the top journal “Advanced Materials†(3).
It is reported that the Gu Yu team is currently in contact with relevant companies to jointly develop this kind of smart patch.
Due to the large number of people with diabetes worldwide and the lack of very good management and treatment methods, academic and industrial circles are very enthusiastic about the development of diabetes management and treatment methods. The psychological needs of non-invasive testing and non-invasive management are also very high.
At present, similar research mainly stays in the pre-clinical animal experiment stage, and it is necessary to improve and optimize the experimental system in different body types of animals. If everything goes well, it will be clinically available in about two or three years, and commercialization in 5-10 years. Therefore, non-invasive diabetes management really goes into life, and you need to wait patiently.
references
1. Lee H, Choi TK, Lee YB, Cho HR, Ghaffari R, et al. 2016. A graphene-based electrochemical device with thermoresponsive microneedles for diabetes monitoring and therapy. Nat Nano advance online publication
2.Yu J, Zhang Y, Ye Y, DiSanto R, Sun W, et al. 2015. Microneedle-array patches loaded with hypoxia-sensitive vesicles provide fast glucose-responsive insulin delivery. Proceedings of the National Academy of Sciences 112:8260 -5
3.Ye Y, Yu J, Wang C, Nguyen NY, Walker GM, et al. 2016. Microneedles Integrated with Pancreatic Cells and Synthetic Glucose-Signal Amplifiers for Smart Insulin Delivery. Advanced Materials: n/an/a
Source: Singularity Network
Medton Medical , https://www.medtonmedical.com